A Simple Guide to Salpingitis
------------------------------
What is Salpingitis?
----------------------
Salpingitis is an acute or chronic infection of the fallopian tubes in females.
What are the causes of Salpingitis?
---------------------------------------
Acute Salpingitis is usually caused by the following:
Infections:
1.sexually transmitted disease like gonorrhea,trichomonas and chlamydia.
2.tuberculosis salpingitis is rare
3.Infection may follow chilbirth or abortion
Mechanical irritants:
intrauterine device may cause acute or chronic Salpingitis
What are the symptoms and signs of Salpingitis?
------------------------------------------------
Persons who has Acute Salpingitis has the following
Symptoms:
1.severe lower abdominal pain
2.purulent vaginal discharge
3.painful or frequency of urination
4.fever
Signs:
1.tenderness in either lower abdominal quadrant
2.discharge can be seen in female vagina
3.vaginal examination - lateral movement of cervix causes pain
- palpation of the fallopian tubes may be very painful
How do you diagnose Salpingitis?
--------------------------------
Diagnosis can usually be made by :
1.History of lower abdominal pain with vaginal discharge
2.Tenderness in lower abdominal region with occasional palpation of tender mass
in the fallopian tube region
3.vaginal examination for tenderness in the tubes region
4.swab to culture for bacteria and sexually transmitted organisms and the antibiotic most appropriate for it.
5.Full blood count
6. endoscopy to examine the fallopian tubes
What are thae complications of Salpingitis?
-------------------------------------------
Acute Salpingitis may progress to chronic Salpingitis:
1. tubal infection with abscess formation(pyosalphinx) or cyst formation(hydrosalphinx)
2. Pelvic abscess
3. Ovarian infection
4.Infertility due to tube blockage
5. Peritonitis may occur with rupture of cyst and abscess
What is the treatment of Salpingitis?
-------------------------------------
1.Approprate Antibiotics for infections especially after uterine bacterial culture
2.Bedrest
3.Surgery may be necessary in cases not responding to antibiotics.
Drainage of the abscess may be done and infected tube resected if necessary
What is the prognosis of Salpingitis?
-------------------------------------------------------
Prognosis is usually good with current antibiotics and medication.
Sexual partner may need to be treated.
Recurrence is quite common.
Infertilty may result in blocked or scarred fallopian tubes
Showing posts with label sexually transmitted disease. Show all posts
Showing posts with label sexually transmitted disease. Show all posts
Monday, June 30, 2008
Friday, March 14, 2008
A Simple Guide to Vulvitis
A Simple Guide to Vulvitis
------------------------------
What is Vulvitis?
----------------------
Vulvitis is an acute inflammation of the vulva in females.
What are the causes of Vulvitis?
---------------------------------------
Vulvitis is usually caused by the following:
Infections:
1.sexually transmitted disease like gonorrhea,trichomonas and chlamydia.
2.Fungal infection such as candidiasis
3.Herpes simplex in recurrent cases
4.Pediculosis pubis or lice
5.pinworm infection in children
6.Urinary infection such as cystitis
Allergies:
1.Clothings
2.perfumes
3.powders
4.drugs
Chemical irritants:
1.vaginal douche
2.detergents used to wash underwear
Mechanical irritants:
1.ill fitting underwear
2.inadequate sexual lubrication
Postmenopausal:
Atrophic vulvovaginitis after menopausal with dryness and inflammation of the vulval and vaginal lining
Generalised disorders:
Dermatological disorders such as lichen simplex
What are the symptoms and signs of Vulvitis?
------------------------------------------------
Persons who has Acute Vulvitis has the following
Symptoms:
1.vulval irritation and itch
2.discharge from vagina
3.painful or frequency of urination
4.excoriation of the inner lining of vulva
Signs:
1.discharge can be seen in female vagina
2.redness and inflammation of the vulva
How do you diagnose Vulvitis?
--------------------------------
Diagnosis can usually be made by :
1.History of vulval itch associated frequency of urination, painful urination or discharge from vagina
2.Vulva shows inflammation, excoriation of lining,
3.Vulval and vaginal swab to culture for bacteria and sexually transmitted organisms and the antibiotic most appropriate for it.
4. biopsy of the suspicious vulval lesions to exclude other causes of vulval problem such as tumor
What is the treatment of Vulvitis?
-------------------------------------
1.Approprate Antibiotics, antifungal for infections especially after urine bacterial culture
2.Antihistamine medicine for itch
3.Topical oestrogen cream for postmenopausal atrophic vulvovaginitis
4.Proper hygience after urination, sexual intercourse and bathing
5.Avoid strong soaps
6.Use of lubricants during sexual intercourse
7.Weight reduction if obese
8.Treat underlying condition such as diabetes,allergic dermatitis,other skin
conditions.
What is the prognosis of Vulvitis?
----------------------------------------
Prognosis is usually good with medication.
Sexual partner may need to be treated.
Recurrence is quite common.
------------------------------
What is Vulvitis?
----------------------
Vulvitis is an acute inflammation of the vulva in females.
What are the causes of Vulvitis?
---------------------------------------
Vulvitis is usually caused by the following:
Infections:
1.sexually transmitted disease like gonorrhea,trichomonas and chlamydia.
2.Fungal infection such as candidiasis
3.Herpes simplex in recurrent cases
4.Pediculosis pubis or lice
5.pinworm infection in children
6.Urinary infection such as cystitis
Allergies:
1.Clothings
2.perfumes
3.powders
4.drugs
Chemical irritants:
1.vaginal douche
2.detergents used to wash underwear
Mechanical irritants:
1.ill fitting underwear
2.inadequate sexual lubrication
Postmenopausal:
Atrophic vulvovaginitis after menopausal with dryness and inflammation of the vulval and vaginal lining
Generalised disorders:
Dermatological disorders such as lichen simplex
What are the symptoms and signs of Vulvitis?
------------------------------------------------
Persons who has Acute Vulvitis has the following
Symptoms:
1.vulval irritation and itch
2.discharge from vagina
3.painful or frequency of urination
4.excoriation of the inner lining of vulva
Signs:
1.discharge can be seen in female vagina
2.redness and inflammation of the vulva
How do you diagnose Vulvitis?
--------------------------------
Diagnosis can usually be made by :
1.History of vulval itch associated frequency of urination, painful urination or discharge from vagina
2.Vulva shows inflammation, excoriation of lining,
3.Vulval and vaginal swab to culture for bacteria and sexually transmitted organisms and the antibiotic most appropriate for it.
4. biopsy of the suspicious vulval lesions to exclude other causes of vulval problem such as tumor
What is the treatment of Vulvitis?
-------------------------------------
1.Approprate Antibiotics, antifungal for infections especially after urine bacterial culture
2.Antihistamine medicine for itch
3.Topical oestrogen cream for postmenopausal atrophic vulvovaginitis
4.Proper hygience after urination, sexual intercourse and bathing
5.Avoid strong soaps
6.Use of lubricants during sexual intercourse
7.Weight reduction if obese
8.Treat underlying condition such as diabetes,allergic dermatitis,other skin
conditions.
What is the prognosis of Vulvitis?
----------------------------------------
Prognosis is usually good with medication.
Sexual partner may need to be treated.
Recurrence is quite common.
Monday, March 10, 2008
A Simple Guide to Urethritis
A Simple Guide to Urethritis
------------------------------
What is Urethritis?
----------------------
Urethritis is an acute infection of the urethra(the tube which allows passage of urine from the bladder to the outside).
What are the causes of Urethritis?
---------------------------------------
Urethritis is usually caused by the following:
1.sexually transmitted disease like gonorrhea and chlamydia.
2.Urinary infection such as cystitis
3.In males associated with prostatitis
4.Urinary stone stuck in the urethra may cause urethitis
6.urinary catheterisation
7.Injury to the urethra
8.Important component of Reiter's Syndrome
What are the symptoms and signs of Urethritis?
------------------------------------------------
Persons who has Acute Urethritis has the following
Symptoms:
------------------
1.painful urination
2.purulent discharge from penis in males or vagina in females
3.frequency of urination
4.cloudy and unpleasant smelling urine, sometimes blood in the urine
5.fever and chills
6.Polyathritis and conjunctivitis in Reiter's Syndrome
Signs:
------
1. pussy discharge can be seen in male's urethra or in female vagina
2.redness and inflammation of the opening of the urethra
How do you diagnose Urethritis?
--------------------------------
Diagnosis can usually be made by :
1.History of sexual activity followed by frequency of urination, painful urination or pussy discharge from urethra or vagina
2.Urine test shows the presence of pus cells, leucocyte, red blood cells and micro-organisms
3.Urine culture for bacteria and sexually transmitted organisms and the antibiotic most appropriate for it.
4. cystoscopy may be necessary to exclude urinary stones,tumours of the bladder in the case of blood in the urine
What is the complications of Urethritis?
-------------------------------------
Upward infections from the urethra can lead to infections of the bladder and kidneys.
What is the treatment of Urethritis?
-------------------------------------
Analgesic medicine for pain
Approprate Antibiotics for infections especially after urine bacterial culture
Lots of fluids
What is the prognosis of Urethritis?
----------------------------------------
Prognosis is usually good with medication.
Sexual partner may need to be treated.
Recurrence is quite common.
------------------------------
What is Urethritis?
----------------------
Urethritis is an acute infection of the urethra(the tube which allows passage of urine from the bladder to the outside).
What are the causes of Urethritis?
---------------------------------------
Urethritis is usually caused by the following:
1.sexually transmitted disease like gonorrhea and chlamydia.
2.Urinary infection such as cystitis
3.In males associated with prostatitis
4.Urinary stone stuck in the urethra may cause urethitis
6.urinary catheterisation
7.Injury to the urethra
8.Important component of Reiter's Syndrome
What are the symptoms and signs of Urethritis?
------------------------------------------------
Persons who has Acute Urethritis has the following
Symptoms:
------------------
1.painful urination
2.purulent discharge from penis in males or vagina in females
3.frequency of urination
4.cloudy and unpleasant smelling urine, sometimes blood in the urine
5.fever and chills
6.Polyathritis and conjunctivitis in Reiter's Syndrome
Signs:
------
1. pussy discharge can be seen in male's urethra or in female vagina
2.redness and inflammation of the opening of the urethra
How do you diagnose Urethritis?
--------------------------------
Diagnosis can usually be made by :
1.History of sexual activity followed by frequency of urination, painful urination or pussy discharge from urethra or vagina
2.Urine test shows the presence of pus cells, leucocyte, red blood cells and micro-organisms
3.Urine culture for bacteria and sexually transmitted organisms and the antibiotic most appropriate for it.
4. cystoscopy may be necessary to exclude urinary stones,tumours of the bladder in the case of blood in the urine
What is the complications of Urethritis?
-------------------------------------
Upward infections from the urethra can lead to infections of the bladder and kidneys.
What is the treatment of Urethritis?
-------------------------------------
Analgesic medicine for pain
Approprate Antibiotics for infections especially after urine bacterial culture
Lots of fluids
What is the prognosis of Urethritis?
----------------------------------------
Prognosis is usually good with medication.
Sexual partner may need to be treated.
Recurrence is quite common.
Thursday, November 15, 2007
A Simple Guide to Trichomoniasis
A Simple Guide to Trichomoniasis
-----------------------------------------
What is Trichomoniasis?
-------------------------------
Trichomoniasis is a common curable sexually transmitted disease caused by the single-celled protozoan parasite, Trichomonas vaginalis.
How is Trichomoniasis spread?
------------------------------------
The parasite is sexually transmitted through penis-to-vagina intercourse with an infected partner.
In women, the vagina is the most common site of infection.
In men the urethra is the most common site of infection.
Women can contract the disease from infected men or women.
Men usually contract it only from infected women.
What are the symptoms of Trichomoniasis?
----------------------------------------------------
Most men with trichomoniasis are symptomless.
Some men may temporarily have an irritation inside the penis, mild discharge, or slight burning after urination or ejaculation.
Women have symptoms of infection which consists of a frothy, yellow-green vaginal discharge with a strong fishy smell.
There may be discomfort during intercourse and urination and irritation and itching of the female genital area.
Cystitis and urethritis can also occur with increased frequency and pain during urination.
Rarely lower abdominal pain can occur.
Pregnant women with trichomoniasis may have babies who are born early or with low birth weight.
How do you diagnose Trichomoniasis?
------------------------------------------------
A physical examination and laboratory test is needed to diagnose trichomoniasis.
The parasite is harder to detect in men than in women.
In women, a pelvic examination can reveal small red ulcerations on the vaginal wall or cervix.
A Pap smear may sometimes show the presence of the trichomonas protozoa.
What is the treatment of Trichomoniasis?
---------------------------------------------------
Trichomoniasis can usually be cured with the prescription drug, metronidazole, given by mouth in a single dose or daily for one week.
It is important for the patient to avoid alcohol with metronidazole and abstain form sex until they and their sex partners complete their treatment and have no symptoms.
Once treated the infection can be cured.
It is important therefore that both partners should be treated at the same time to eliminate the parasite.
Metronidazole can be used to treat pregnant women.
Having trichomoniasis once does not protect a person from getting it again. Following successful treatment, people can still be susceptible to re-infection.
How do you prevent Trichomoniasis?
---------------------------------------------
The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual contact.
A long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected is important.
Latex male condoms, when used consistently and correctly, can reduce the risk of transmission of trichomoniasis.
A person diagnosed with trichomoniasis (or any other STD) should receive treatment and should notify all recent sex partners so that they can be treated. This reduces the risk that the sex partners will develop complications from trichomoniasis and reduces the risk that the person with trichomoniasis will become re-infected.
Sex should be stopped until the person with trichomoniasis and all of his or her recent partners complete treatment for trichomoniasis and have no symptoms.
There is no vaccine for Trichomoniasis.
-----------------------------------------
What is Trichomoniasis?
-------------------------------
Trichomoniasis is a common curable sexually transmitted disease caused by the single-celled protozoan parasite, Trichomonas vaginalis.
How is Trichomoniasis spread?
------------------------------------
The parasite is sexually transmitted through penis-to-vagina intercourse with an infected partner.
In women, the vagina is the most common site of infection.
In men the urethra is the most common site of infection.
Women can contract the disease from infected men or women.
Men usually contract it only from infected women.
What are the symptoms of Trichomoniasis?
----------------------------------------------------
Most men with trichomoniasis are symptomless.
Some men may temporarily have an irritation inside the penis, mild discharge, or slight burning after urination or ejaculation.
Women have symptoms of infection which consists of a frothy, yellow-green vaginal discharge with a strong fishy smell.
There may be discomfort during intercourse and urination and irritation and itching of the female genital area.
Cystitis and urethritis can also occur with increased frequency and pain during urination.
Rarely lower abdominal pain can occur.
Pregnant women with trichomoniasis may have babies who are born early or with low birth weight.
How do you diagnose Trichomoniasis?
------------------------------------------------
A physical examination and laboratory test is needed to diagnose trichomoniasis.
The parasite is harder to detect in men than in women.
In women, a pelvic examination can reveal small red ulcerations on the vaginal wall or cervix.
A Pap smear may sometimes show the presence of the trichomonas protozoa.
What is the treatment of Trichomoniasis?
---------------------------------------------------
Trichomoniasis can usually be cured with the prescription drug, metronidazole, given by mouth in a single dose or daily for one week.
It is important for the patient to avoid alcohol with metronidazole and abstain form sex until they and their sex partners complete their treatment and have no symptoms.
Once treated the infection can be cured.
It is important therefore that both partners should be treated at the same time to eliminate the parasite.
Metronidazole can be used to treat pregnant women.
Having trichomoniasis once does not protect a person from getting it again. Following successful treatment, people can still be susceptible to re-infection.
How do you prevent Trichomoniasis?
---------------------------------------------
The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual contact.
A long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected is important.
Latex male condoms, when used consistently and correctly, can reduce the risk of transmission of trichomoniasis.
A person diagnosed with trichomoniasis (or any other STD) should receive treatment and should notify all recent sex partners so that they can be treated. This reduces the risk that the sex partners will develop complications from trichomoniasis and reduces the risk that the person with trichomoniasis will become re-infected.
Sex should be stopped until the person with trichomoniasis and all of his or her recent partners complete treatment for trichomoniasis and have no symptoms.
There is no vaccine for Trichomoniasis.
Monday, November 12, 2007
A Simple Guide to Gonorrhea
A Simple Guide to Gonorrhea
-----------------------------------
What is Gonorrhea?
------------------------
Gonorrhea is a sexually transmitted disease caused by the gram negative bacteria Neisseria gonorrhoeae.
How is gonorrhea spread?
-----------------------------
Gonorrhea is a very common infectious disease, a bacterium that can grow and multiply easily in the warm, moist areas of the reproductive tract, including the cervix, uterus and fallopian tubes in women, and in the urethra in women and men.
The bacterium can also grow in the mouth, throat, eyes, and anus.
Gonorrhea is spread by infected people through contact with the penis, vagina, mouth, or anus.
There is no life long immunity after tratment with Gonorrhea.
A person who has been treated for gonorrhea may get infected again if there is sexual contact with a person infected with gonorrhea.
Gonorrhea can also be spread from mother to baby during delivery.
Who is at risk for gonorrhea?
-----------------------------------
Any sexually active person can be infected with gonorrhea if their partner has the disease.
What are the symptoms of gonorrhea?
---------------------------------------------
A high percentage of men with gonorrhea do not have any symptoms at all.
Some men have some symptoms that appear two to five days after infection.
Symptoms include
1.a burning sensation when urinating, or a white, yellow, or green discharge from the penis.
2. painful or swollen testicles.
In women the symptoms of gonorrhea are often mild.
Most women who are infected have no symptoms.
The initial symptoms in women include
1.a painful or burning sensation when urinating,
2.increased vaginal discharge,
3.vaginal bleeding between periods.
4.lower abdominal pain due to salpingitis(infected fallopian tubes)
Women with gonorrhea are at risk of developing serious complications from the infection.
Symptoms of rectal infection in both men and women may include discharge, anal itching, soreness, bleeding, or painful bowel movements.
Most of the time rectal infection do not cause symptoms.
Infections in the throat may cause a sore throat.
Usually there are no symptoms.
How does gonorrhea affect a pregnant woman and her baby?
-----------------------------------------------------------------------
A pregnant woman with gonorrhea may give the infection to her baby as the baby passes through the birth canal during delivery.
This can cause blindness, joint infection, or a life-threatening blood infection in the baby.
Treatment of gonorrhea should be started as soon as it is detected in pregnant women.
How is gonorrhea diagnosed?
-----------------------------------
There are several laboratory tests available to diagnose gonorrhea:
1. a swab may be taken from cervix, urethra, rectum, or throat for testing
2. A direct Gram smear test of a sample from a urethra or a cervix allows the doctor in the clinic to see the gonorrhea bacterium under a microscope.
3. blood test can also detect the presence of gonorrhea in the blood stream
What is the treatment for gonorrhea?
--------------------------------------------
There are several antibiotics(penicillin, tetracyclines, spectinomycin) which can successfully cure gonorrhea in adolescents and adults.
Drug-resistant strains of gonorrhea are increasing in many areas of the world and successful treatment of gonorrhea is becoming more difficult.
Sometimes people with gonorrhea also have chlamydia.
Antibiotics for both infections are usually given together.
Persons with gonorrhea should be tested for other STDs.
It is advisable to take all of the medication prescribed to cure gonorrhea.
People who have had gonorrhea and have been treated can get the disease a second time if they have sexual contact with persons infected with gonorrhea.
What are the complications of gonorrhea?
--------------------------------------------------
Untreated gonorrhea can cause serious and permanent complications in both women and men.
In women, gonorrhea is a common cause of pelvic inflammatory disease (PID).
Women with PID may not have symptoms.
Symptoms when present can be very severe and can include abdominal pain and fever.
PID can cause internal abscesses in the pelvis which can give rise to long-lasting, chronic pelvic pain.
PID can damage the fallopian tubes enough to cause infertility and the risk of ectopic pregnancy.
Ectopic pregnancy is a life-threatening condition in which a fertilized egg grows outside the uterus, usually in a fallopian tube, sometimes in the abdomen.
In men gonorrhea can cause epididymitis, a painful infection of the testicles that can lead to infertility if left untreated.
Prostatits(infection of prostate), seminal vesiculitis and chronic urethral infection may be associated with fever and lead to urethral strictures causing difficulty in passing urine.
People with gonorrhea are more likely to contract HIV the virus that causes AIDS.
Gonorrhea can spread to the blood, joints or eyes(uveitis).
Blood infection or septicemia can be life threatening.
How can gonorrhea be prevented?
-----------------------------------------
The best way to avoid transmission of sexually transmitted diseases is to abstain from sexual intercourse.
He or she should be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Latex condoms, when used consistently and correctly, can reduce the risk of transmission of gonorrhea.
Any genital symptoms such as discharge or burning sensation during urination or unusual sore or rash should be a signal to stop having sex.
A person who has been diagnosed and treated for gonorrhea should notify all recent sex partners so they can also be treated.
In this way there is less risk that the sexual partners will develop serious complications from gonorrhea.
It will also reduce the person's risk of becoming re-infected.
The person and all of his or her sex partners must avoid sex until they have completed their treatment for gonorrhea.
-----------------------------------
What is Gonorrhea?
------------------------
Gonorrhea is a sexually transmitted disease caused by the gram negative bacteria Neisseria gonorrhoeae.
How is gonorrhea spread?
-----------------------------
Gonorrhea is a very common infectious disease, a bacterium that can grow and multiply easily in the warm, moist areas of the reproductive tract, including the cervix, uterus and fallopian tubes in women, and in the urethra in women and men.
The bacterium can also grow in the mouth, throat, eyes, and anus.
Gonorrhea is spread by infected people through contact with the penis, vagina, mouth, or anus.
There is no life long immunity after tratment with Gonorrhea.
A person who has been treated for gonorrhea may get infected again if there is sexual contact with a person infected with gonorrhea.
Gonorrhea can also be spread from mother to baby during delivery.
Who is at risk for gonorrhea?
-----------------------------------
Any sexually active person can be infected with gonorrhea if their partner has the disease.
What are the symptoms of gonorrhea?
---------------------------------------------
A high percentage of men with gonorrhea do not have any symptoms at all.
Some men have some symptoms that appear two to five days after infection.
Symptoms include
1.a burning sensation when urinating, or a white, yellow, or green discharge from the penis.
2. painful or swollen testicles.
In women the symptoms of gonorrhea are often mild.
Most women who are infected have no symptoms.
The initial symptoms in women include
1.a painful or burning sensation when urinating,
2.increased vaginal discharge,
3.vaginal bleeding between periods.
4.lower abdominal pain due to salpingitis(infected fallopian tubes)
Women with gonorrhea are at risk of developing serious complications from the infection.
Symptoms of rectal infection in both men and women may include discharge, anal itching, soreness, bleeding, or painful bowel movements.
Most of the time rectal infection do not cause symptoms.
Infections in the throat may cause a sore throat.
Usually there are no symptoms.
How does gonorrhea affect a pregnant woman and her baby?
-----------------------------------------------------------------------
A pregnant woman with gonorrhea may give the infection to her baby as the baby passes through the birth canal during delivery.
This can cause blindness, joint infection, or a life-threatening blood infection in the baby.
Treatment of gonorrhea should be started as soon as it is detected in pregnant women.
How is gonorrhea diagnosed?
-----------------------------------
There are several laboratory tests available to diagnose gonorrhea:
1. a swab may be taken from cervix, urethra, rectum, or throat for testing
2. A direct Gram smear test of a sample from a urethra or a cervix allows the doctor in the clinic to see the gonorrhea bacterium under a microscope.
3. blood test can also detect the presence of gonorrhea in the blood stream
What is the treatment for gonorrhea?
--------------------------------------------
There are several antibiotics(penicillin, tetracyclines, spectinomycin) which can successfully cure gonorrhea in adolescents and adults.
Drug-resistant strains of gonorrhea are increasing in many areas of the world and successful treatment of gonorrhea is becoming more difficult.
Sometimes people with gonorrhea also have chlamydia.
Antibiotics for both infections are usually given together.
Persons with gonorrhea should be tested for other STDs.
It is advisable to take all of the medication prescribed to cure gonorrhea.
People who have had gonorrhea and have been treated can get the disease a second time if they have sexual contact with persons infected with gonorrhea.
What are the complications of gonorrhea?
--------------------------------------------------
Untreated gonorrhea can cause serious and permanent complications in both women and men.
In women, gonorrhea is a common cause of pelvic inflammatory disease (PID).
Women with PID may not have symptoms.
Symptoms when present can be very severe and can include abdominal pain and fever.
PID can cause internal abscesses in the pelvis which can give rise to long-lasting, chronic pelvic pain.
PID can damage the fallopian tubes enough to cause infertility and the risk of ectopic pregnancy.
Ectopic pregnancy is a life-threatening condition in which a fertilized egg grows outside the uterus, usually in a fallopian tube, sometimes in the abdomen.
In men gonorrhea can cause epididymitis, a painful infection of the testicles that can lead to infertility if left untreated.
Prostatits(infection of prostate), seminal vesiculitis and chronic urethral infection may be associated with fever and lead to urethral strictures causing difficulty in passing urine.
People with gonorrhea are more likely to contract HIV the virus that causes AIDS.
Gonorrhea can spread to the blood, joints or eyes(uveitis).
Blood infection or septicemia can be life threatening.
How can gonorrhea be prevented?
-----------------------------------------
The best way to avoid transmission of sexually transmitted diseases is to abstain from sexual intercourse.
He or she should be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Latex condoms, when used consistently and correctly, can reduce the risk of transmission of gonorrhea.
Any genital symptoms such as discharge or burning sensation during urination or unusual sore or rash should be a signal to stop having sex.
A person who has been diagnosed and treated for gonorrhea should notify all recent sex partners so they can also be treated.
In this way there is less risk that the sexual partners will develop serious complications from gonorrhea.
It will also reduce the person's risk of becoming re-infected.
The person and all of his or her sex partners must avoid sex until they have completed their treatment for gonorrhea.
Friday, November 9, 2007
A Simple Guide to Genital Herpes
A Simple Guide to Genital Herpes
----------------------------------------
What is Genital Herpes?
-----------------------------
Genital herpes is a sexually transmitted disease caused by the herpes simplex viruses type 1 (HSV-1) and type 2 (HSV-2).
Most genital herpes is caused by HSV-2.
Incubation peroid is 14 days to several weeks.
What are the symptoms of Genital Herpes?
--------------------------------------------------
Most infected patients do not have any signs or symptoms from Genital herpes infection.
In the male, small blisters occur on the penis glans and on both of the scrotums.
If the urethra is involved. there may be discharge and pain on urination.
In the female, there may be one or more blisters on or around the genitals or rectum. The blisters normally break, leaving painful ulcers which may take two to four weeks to heal.
Typically, recurrence of the blisters may appear weeks or months after the first and is usually less severe and shorter than the first outbreak.
The infection can stay in the body indefinitely with the number of outbreaks decreasing over a period of years.
How is Genital Herpes spread?
-------------------------------------
Genital herpes is usaully a sexually transmitted disease.
Genital HSV-2 infection is more common in women (25%) than in men (20%).
This may be due to male-to-female transmissions.
HSV-1 and HSV-2 viruses can be found in and released from the blisters and ulcers that the viruses cause.
They also are released between outbreaks from skin that does not appear to be broken or to have a sore.
Transmission can occur from an infected partner who does not have a visible sore and may not know that he or she is infected.
HSV-1 can also cause genital herpes.
It however causes more infections of the mouth and lips, so-called "cold sores."
HSV-1 infection of the genitals can be caused by oral-genital or genital-genital contact with a person who has HSV-1 infection.
Genital HSV-1 outbreaks does not recur as often as genital HSV-2 outbreaks.
How do you diagnose Genital Herpes?
--------------------------------------------
The signs and symptoms of HSV-2 infection may be none to obvious.
Doctors can diagnose genital herpes by visual examination if the outbreak is typical and by taking a sample from the sores and testing it in a laboratory.
HSV infections can be difficult to diagnose between outbreaks.
The best way to confirm the presence of Genital herpes is to do a blood test for HSV1 and HSV2 viruses. The results however may not 100% accurate.
Most people infected with genital herpes do not know of their infection.
Once the virus is transmitted, an outbreak usually occurs within two weeks and the sores typically heal within two to four weeks.
During the primary episode, signs and symptoms may include a second episode of sores and sometimes fever and swollen glands.
Most individuals with HSV-2 infection do not have sores, or the sores may be so mild that they do not even notice.
Most people diagnosed with a first episode of genital herpes can expect to have several symptomatic recurrences within a year.
Usually these recurrences decrease in frequency.
What is the treatment of Genital Herpes?
-------------------------------------------------
There is no treatment that can cure herpes but antiviral medications like acyclovir can shorten and prevent outbreaks during the period of time the person takes the medication.
In addition the medications can reduce transmission to partners.
How do you prevent Genital Herpes?
-------------------------------------------
1.abstainance from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected from genital herpes.
2.protection using a latex condom during sexual contact. However since a condom may not cover all infected areas, even correct and consistent use of latex condoms cannot guarantee protection from genital herpes.
3.Persons with herpes should abstain from sexual activity with uninfected partners.
This is a very important moral responsibility.
Sex partners of infected persons should be advised that they may become infected.
Sex partners can seek testing to determine if they are infected with HSV.
A positive HSV-2 blood test most likely indicates a genital herpes infection.
What are the Complications of Genital herpes?
--------------------------------------------------------
1.In some cases, genital herpes can cause recurrent painful genital sores in many adults.
2.Herpes infection can be severe in people with suppressed immune systems eg. HIV.
3.psychological distress may occur in people who know they are infected because the herpes is not curable.
4.genital HSV can cause potentially fatal infections in babies.
If a woman has active genital herpes at delivery, a cesarean delivery is usually performed.
Infection of a baby from a woman with herpes infection fortunately is rare.
5.Herpes may play a role in the spread of HIV the virus that causes AIDS. Herpes can make people more susceptible to HIV infection, and it can make HIV-infected individuals more infectious to others.
----------------------------------------
What is Genital Herpes?
-----------------------------
Genital herpes is a sexually transmitted disease caused by the herpes simplex viruses type 1 (HSV-1) and type 2 (HSV-2).
Most genital herpes is caused by HSV-2.
Incubation peroid is 14 days to several weeks.
What are the symptoms of Genital Herpes?
--------------------------------------------------
Most infected patients do not have any signs or symptoms from Genital herpes infection.
In the male, small blisters occur on the penis glans and on both of the scrotums.
If the urethra is involved. there may be discharge and pain on urination.
In the female, there may be one or more blisters on or around the genitals or rectum. The blisters normally break, leaving painful ulcers which may take two to four weeks to heal.
Typically, recurrence of the blisters may appear weeks or months after the first and is usually less severe and shorter than the first outbreak.
The infection can stay in the body indefinitely with the number of outbreaks decreasing over a period of years.
How is Genital Herpes spread?
-------------------------------------
Genital herpes is usaully a sexually transmitted disease.
Genital HSV-2 infection is more common in women (25%) than in men (20%).
This may be due to male-to-female transmissions.
HSV-1 and HSV-2 viruses can be found in and released from the blisters and ulcers that the viruses cause.
They also are released between outbreaks from skin that does not appear to be broken or to have a sore.
Transmission can occur from an infected partner who does not have a visible sore and may not know that he or she is infected.
HSV-1 can also cause genital herpes.
It however causes more infections of the mouth and lips, so-called "cold sores."
HSV-1 infection of the genitals can be caused by oral-genital or genital-genital contact with a person who has HSV-1 infection.
Genital HSV-1 outbreaks does not recur as often as genital HSV-2 outbreaks.
How do you diagnose Genital Herpes?
--------------------------------------------
The signs and symptoms of HSV-2 infection may be none to obvious.
Doctors can diagnose genital herpes by visual examination if the outbreak is typical and by taking a sample from the sores and testing it in a laboratory.
HSV infections can be difficult to diagnose between outbreaks.
The best way to confirm the presence of Genital herpes is to do a blood test for HSV1 and HSV2 viruses. The results however may not 100% accurate.
Most people infected with genital herpes do not know of their infection.
Once the virus is transmitted, an outbreak usually occurs within two weeks and the sores typically heal within two to four weeks.
During the primary episode, signs and symptoms may include a second episode of sores and sometimes fever and swollen glands.
Most individuals with HSV-2 infection do not have sores, or the sores may be so mild that they do not even notice.
Most people diagnosed with a first episode of genital herpes can expect to have several symptomatic recurrences within a year.
Usually these recurrences decrease in frequency.
What is the treatment of Genital Herpes?
-------------------------------------------------
There is no treatment that can cure herpes but antiviral medications like acyclovir can shorten and prevent outbreaks during the period of time the person takes the medication.
In addition the medications can reduce transmission to partners.
How do you prevent Genital Herpes?
-------------------------------------------
1.abstainance from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected from genital herpes.
2.protection using a latex condom during sexual contact. However since a condom may not cover all infected areas, even correct and consistent use of latex condoms cannot guarantee protection from genital herpes.
3.Persons with herpes should abstain from sexual activity with uninfected partners.
This is a very important moral responsibility.
Sex partners of infected persons should be advised that they may become infected.
Sex partners can seek testing to determine if they are infected with HSV.
A positive HSV-2 blood test most likely indicates a genital herpes infection.
What are the Complications of Genital herpes?
--------------------------------------------------------
1.In some cases, genital herpes can cause recurrent painful genital sores in many adults.
2.Herpes infection can be severe in people with suppressed immune systems eg. HIV.
3.psychological distress may occur in people who know they are infected because the herpes is not curable.
4.genital HSV can cause potentially fatal infections in babies.
If a woman has active genital herpes at delivery, a cesarean delivery is usually performed.
Infection of a baby from a woman with herpes infection fortunately is rare.
5.Herpes may play a role in the spread of HIV the virus that causes AIDS. Herpes can make people more susceptible to HIV infection, and it can make HIV-infected individuals more infectious to others.
Tuesday, November 6, 2007
A Simple Guide to Hepatitis B
A Simple Guide to Hepatitis B
------------------------------------
What is Hepatitis B?-
-------------------------
Hepatitis B is a serious chronic inflammatory liver disease caused by a virus which is called hepatitis B virus (HBV).
What are the Symptoms of Hepatitis B?
----------------------------------------------
Most of the time a person with HBV infection has no symptoms at all.
Older people are more likely to have symptoms.
If you have symptoms, they might include :
1.jaundice (yellowing of the skin and white of eye)
2.dark coloured urine
3.pale stools
4.prolonged tiredness
5.nausea and vomiting.
6.loss of appetite
7.abdominal pain
8.fever and joint pains
How is the diagnosis of Hepatitis made?
-----------------------------------------------
A blood test is the only way to diagnose hepatitis B.
You may be infected with HBV and may even spread it to others without knowing it.
HBV can be spread from an infected mother to her infant during birth.
To prevent spread of HBV from infected mothers to their infants, every woman should have her blood tested for hepatitis B surface antigen (HBsAg) during each pregnancy.
What is the treatment of Hepatitis B?
-------------------------------------------
There are no medications available for recently acquired (acute) HBV infection. There are antiviral drugs eg interferon which may be able to treat chronic HBV infection.
Who is at risk of getting Hepatitis B?
-------------------------------------------
For those who has never been immunised or do not have antibodies from having a previous Hepatitis B infection, you are at risk of Hepatitis B infection.
The Hepatitis B virus is is not spread through food or water, sharing eating utensils, breastfeeding, hugging, coughing, sneezing, or skin contact.
HBV is spread by exposure to infected blood from skin puncture or contact with mucous membranes.
It is spread by:
1.sexual contact with an infected person
2.an infected mother to her newborn during childbirth
3.a Hepatitis B infected person's blood during blood transfusion
4.sharing of injection needles among drug abusers
5.accidental cuts to the skin by a nail clipper, shaving blade or other instruments that are contaminated with a Hepatitis B infected person's blood
6.contact with an infected person's saliva or blood through cuts or sores in the mouth or skin. Kissing by itself do not spread HBV unless there is a cut in the lips.
7.during acupuncture, body or ear piercing and tattooing if the needles used are contaminated with Hepatitis B infected person's blood
8.have a job that involves contact with human blood or body fluids
What is the best prevention for Hepatitis B?
----------------------------------------------------
Hepatitis B vaccine is the best prevention against hepatitis B.
If you do not have antibodies from a previous infection and if you are not a Hepatitis B carrier, you can get vaccinated against Hepatitis B and protect yourself from its complications.
Hepatitis B vaccine is recommended for all infants, for children and adolescents who were not vaccinated as infants, and for all unvaccinated adults who are at risk for HBV infection as well as any adult who wants to be protected against HBV infection.
The vaccine is safe.
It is also extremely effective provided you complete all 3 doses:
1st dose - at the appointed date
2nd dose - 1 month after the 1st dose
3rd dose - 5 months after the 2nd dose
A booster vaccination may be necessary after 5 years if the blood test showed a drop in immunity.
Infants born to infected mothers need to get hepatitis B vaccine and another shot call HBIG (hepatitis B immune globulin) soon after birth to prevent infection.
Besides vaccination, other ways to prevent transmission of HBV are:
1.avoid multiple sexual partners; keep to one sexual partner
2.Latex condoms, when used consistently and correctly, may reduce the risk of sexually transmitted HBV transmission.
3.Do not inject illegal drugs. Never share needles, syringes or drugs.
4.Do not share personal items like razors, toothbrushes or any other instruments that may cause tears to the skin and hence spread of any blood borne infection.
5.seek reliable operators for ear or body piercing, tattooing or acupuncture.
What happens if I am a Hepatitis B carrier?
--------------------------------------------------
A simple blood test can tell if you are a carrier, are immune or need immunisation.
If you are found to be a carrier, then:
1.you will need to see your doctor every 6 months to a year for tests to check your liver function and blood alpha-foetoprotein which is a cancer marker for liver cancer
2.your immediate family members should go for blood tests.
They should get immunised if they are not immune.
If they are carriers too, they should go for regular follow up with the doctor.
3.you should take precautions to prevent the spread of hepatitis B to your family and loved ones
4.you should avoid smoking and drinking alcohol as they may further increase the risk of damage to your liver
5.inform your doctor and dentist that you are a carrier
6.do not donate blood, organs or sperm
7.know the symptoms and signs of the various complications and see your doctor at once if you experience any of them.
What are the Complications of Hepatitis B ?
---------------------------------------------------
Hepatitis B can lead to complications like:
1.acute hepatitis (episode of liver inflammation)
2.chronic hepatitis (permanent liver inflammation)
3.liver cirrhosis (permanent scarring and hardening of the liver)
4.liver failure (liver is unable to function,
resulting in toxins accumulating in body)
5.liver cancer
Those who recover completely from Hepatitis B infection become immune to the disease.
1 in 10 people who get infected with the virus become carriers who then carries the Hepatitis B virus permanently in his body.
Hepatitis B carriers seldom show any symptoms but they can:
1.spread the disease to others
2.develop serious liver complications such as those mentioned above.
About 15%-25% of people with chronic HBV infection die prematurely from these complications.
------------------------------------
What is Hepatitis B?-
-------------------------
Hepatitis B is a serious chronic inflammatory liver disease caused by a virus which is called hepatitis B virus (HBV).
What are the Symptoms of Hepatitis B?
----------------------------------------------
Most of the time a person with HBV infection has no symptoms at all.
Older people are more likely to have symptoms.
If you have symptoms, they might include :
1.jaundice (yellowing of the skin and white of eye)
2.dark coloured urine
3.pale stools
4.prolonged tiredness
5.nausea and vomiting.
6.loss of appetite
7.abdominal pain
8.fever and joint pains
How is the diagnosis of Hepatitis made?
-----------------------------------------------
A blood test is the only way to diagnose hepatitis B.
You may be infected with HBV and may even spread it to others without knowing it.
HBV can be spread from an infected mother to her infant during birth.
To prevent spread of HBV from infected mothers to their infants, every woman should have her blood tested for hepatitis B surface antigen (HBsAg) during each pregnancy.
What is the treatment of Hepatitis B?
-------------------------------------------
There are no medications available for recently acquired (acute) HBV infection. There are antiviral drugs eg interferon which may be able to treat chronic HBV infection.
Who is at risk of getting Hepatitis B?
-------------------------------------------
For those who has never been immunised or do not have antibodies from having a previous Hepatitis B infection, you are at risk of Hepatitis B infection.
The Hepatitis B virus is is not spread through food or water, sharing eating utensils, breastfeeding, hugging, coughing, sneezing, or skin contact.
HBV is spread by exposure to infected blood from skin puncture or contact with mucous membranes.
It is spread by:
1.sexual contact with an infected person
2.an infected mother to her newborn during childbirth
3.a Hepatitis B infected person's blood during blood transfusion
4.sharing of injection needles among drug abusers
5.accidental cuts to the skin by a nail clipper, shaving blade or other instruments that are contaminated with a Hepatitis B infected person's blood
6.contact with an infected person's saliva or blood through cuts or sores in the mouth or skin. Kissing by itself do not spread HBV unless there is a cut in the lips.
7.during acupuncture, body or ear piercing and tattooing if the needles used are contaminated with Hepatitis B infected person's blood
8.have a job that involves contact with human blood or body fluids
What is the best prevention for Hepatitis B?
----------------------------------------------------
Hepatitis B vaccine is the best prevention against hepatitis B.
If you do not have antibodies from a previous infection and if you are not a Hepatitis B carrier, you can get vaccinated against Hepatitis B and protect yourself from its complications.
Hepatitis B vaccine is recommended for all infants, for children and adolescents who were not vaccinated as infants, and for all unvaccinated adults who are at risk for HBV infection as well as any adult who wants to be protected against HBV infection.
The vaccine is safe.
It is also extremely effective provided you complete all 3 doses:
1st dose - at the appointed date
2nd dose - 1 month after the 1st dose
3rd dose - 5 months after the 2nd dose
A booster vaccination may be necessary after 5 years if the blood test showed a drop in immunity.
Infants born to infected mothers need to get hepatitis B vaccine and another shot call HBIG (hepatitis B immune globulin) soon after birth to prevent infection.
Besides vaccination, other ways to prevent transmission of HBV are:
1.avoid multiple sexual partners; keep to one sexual partner
2.Latex condoms, when used consistently and correctly, may reduce the risk of sexually transmitted HBV transmission.
3.Do not inject illegal drugs. Never share needles, syringes or drugs.
4.Do not share personal items like razors, toothbrushes or any other instruments that may cause tears to the skin and hence spread of any blood borne infection.
5.seek reliable operators for ear or body piercing, tattooing or acupuncture.
What happens if I am a Hepatitis B carrier?
--------------------------------------------------
A simple blood test can tell if you are a carrier, are immune or need immunisation.
If you are found to be a carrier, then:
1.you will need to see your doctor every 6 months to a year for tests to check your liver function and blood alpha-foetoprotein which is a cancer marker for liver cancer
2.your immediate family members should go for blood tests.
They should get immunised if they are not immune.
If they are carriers too, they should go for regular follow up with the doctor.
3.you should take precautions to prevent the spread of hepatitis B to your family and loved ones
4.you should avoid smoking and drinking alcohol as they may further increase the risk of damage to your liver
5.inform your doctor and dentist that you are a carrier
6.do not donate blood, organs or sperm
7.know the symptoms and signs of the various complications and see your doctor at once if you experience any of them.
What are the Complications of Hepatitis B ?
---------------------------------------------------
Hepatitis B can lead to complications like:
1.acute hepatitis (episode of liver inflammation)
2.chronic hepatitis (permanent liver inflammation)
3.liver cirrhosis (permanent scarring and hardening of the liver)
4.liver failure (liver is unable to function,
resulting in toxins accumulating in body)
5.liver cancer
Those who recover completely from Hepatitis B infection become immune to the disease.
1 in 10 people who get infected with the virus become carriers who then carries the Hepatitis B virus permanently in his body.
Hepatitis B carriers seldom show any symptoms but they can:
1.spread the disease to others
2.develop serious liver complications such as those mentioned above.
About 15%-25% of people with chronic HBV infection die prematurely from these complications.
Tuesday, October 9, 2007
A Simple Guide to Chlamydia
A Simple Guide to Chlamydia
-----------------------------------
What is Chlamydia?
------------------------
Chlamydia is a bacterial infection which is one of the most common sexually transmitted diseases.
It used to be called Lymphogranuloma venereum because of the typically enlarged lymph nodes at the groins.
It can lead to pelvic inflammatory disease (PID), as well as sterility and pregnancy problems.
How do you get Chlamydia?
--------------------------------
Chlamydia is highly contagious.
It spreads by sexual contact with an infected partner.
It can also be transmitted from mother to child during birth.
This may lead to an infection of the eyes and lungs in the infant.
It is also be transmitted through casual sexual contact with other people.
What are the signs & symptoms of Chlamydia?
------------------------------------------------------
About 80% of women and 10% of men display no symptoms.
For the rest the symptoms often appear 7-14 days after transmission in the following ways:
For men:
1.Discharge from a papule on the penis
2.Burning pain and itching when urinating.
3.lymph nodes enlargement at inguinal regions
4. Anal infections in homosexuals
Symptoms present early a few days after exposure, go away, only to return.
Advanced Chlamydia infection may lead to inflammation of the sperm duct (epididymitis), proctitis (anal region) and sterility.
For women:
1.Vaginal itching or discharge.
2.Abdominal pain,
3.Bleeding between menstrual periods
4.Low grade fever
5.Anal infections
The disease can also cause cervicitis, endometritis and pelvic inflammatory disease which can result in sterility.
For infants:
1.Fever
2.Pneumonia
3.Conjunctivitis
Symptoms usually show up one week to one month after exposure.
Besides the above symptoms, headache, conjunctivitis, skin rashes, nausea and vomiting can be present.
How can Chlamydia be detected?
---------------------------------------
Women may be tested through the insertion of a swab into the cervix during a pelvic exam.
Men can be examined by inserting a swab into the urethra to take a specimen.
Urine testing can also be done for both sexes.
Blood test for chlamydia can also be done.
What is the Treatment of Chlamydia?
--------------------------------------------
Early treatment is important as it can protect against problems like pelvic inflammatory disease as well as sterility and pregnancy problems.
Patients typically undergo antibiotic treatment (usually tetracycline or sulphonamides) for a week.
The medication can be taken orally.
This treatment must be followed through even when symptoms of Chlamydia disappear.
Alcohol should be avoided when taking antibiotics, as well as milk and other dairy products.
Where Chlamydia has been transmitted through sexual contact, it is essential that both sexual partners are treated for the disease.
It is recommended that both partners abstain from sexual activity from the time of diagnosis until they have completed treatment.
Follow-up treatment is also important, as doctors need to make sure the infection has been cured.
How can I avoid contracting Chlamydia?
------------------------------------------------
The best way to prevent Chlamydia is through improved hygiene standards and lifestyle changes.
Sexually active persons should use condoms.
Abstinence is recommended for those infected and on antibiotic treatment.
One's risk for Chlamydia, or any other sexually transmitted disease, increases with the number of sexual partners.
Prevention is always better than cure!
-----------------------------------
What is Chlamydia?
------------------------
Chlamydia is a bacterial infection which is one of the most common sexually transmitted diseases.
It used to be called Lymphogranuloma venereum because of the typically enlarged lymph nodes at the groins.
It can lead to pelvic inflammatory disease (PID), as well as sterility and pregnancy problems.
How do you get Chlamydia?
--------------------------------
Chlamydia is highly contagious.
It spreads by sexual contact with an infected partner.
It can also be transmitted from mother to child during birth.
This may lead to an infection of the eyes and lungs in the infant.
It is also be transmitted through casual sexual contact with other people.
What are the signs & symptoms of Chlamydia?
------------------------------------------------------
About 80% of women and 10% of men display no symptoms.
For the rest the symptoms often appear 7-14 days after transmission in the following ways:
For men:
1.Discharge from a papule on the penis
2.Burning pain and itching when urinating.
3.lymph nodes enlargement at inguinal regions
4. Anal infections in homosexuals
Symptoms present early a few days after exposure, go away, only to return.
Advanced Chlamydia infection may lead to inflammation of the sperm duct (epididymitis), proctitis (anal region) and sterility.
For women:
1.Vaginal itching or discharge.
2.Abdominal pain,
3.Bleeding between menstrual periods
4.Low grade fever
5.Anal infections
The disease can also cause cervicitis, endometritis and pelvic inflammatory disease which can result in sterility.
For infants:
1.Fever
2.Pneumonia
3.Conjunctivitis
Symptoms usually show up one week to one month after exposure.
Besides the above symptoms, headache, conjunctivitis, skin rashes, nausea and vomiting can be present.
How can Chlamydia be detected?
---------------------------------------
Women may be tested through the insertion of a swab into the cervix during a pelvic exam.
Men can be examined by inserting a swab into the urethra to take a specimen.
Urine testing can also be done for both sexes.
Blood test for chlamydia can also be done.
What is the Treatment of Chlamydia?
--------------------------------------------
Early treatment is important as it can protect against problems like pelvic inflammatory disease as well as sterility and pregnancy problems.
Patients typically undergo antibiotic treatment (usually tetracycline or sulphonamides) for a week.
The medication can be taken orally.
This treatment must be followed through even when symptoms of Chlamydia disappear.
Alcohol should be avoided when taking antibiotics, as well as milk and other dairy products.
Where Chlamydia has been transmitted through sexual contact, it is essential that both sexual partners are treated for the disease.
It is recommended that both partners abstain from sexual activity from the time of diagnosis until they have completed treatment.
Follow-up treatment is also important, as doctors need to make sure the infection has been cured.
How can I avoid contracting Chlamydia?
------------------------------------------------
The best way to prevent Chlamydia is through improved hygiene standards and lifestyle changes.
Sexually active persons should use condoms.
Abstinence is recommended for those infected and on antibiotic treatment.
One's risk for Chlamydia, or any other sexually transmitted disease, increases with the number of sexual partners.
Prevention is always better than cure!
Wednesday, September 19, 2007
A Simple Guide to Cervical Cancer
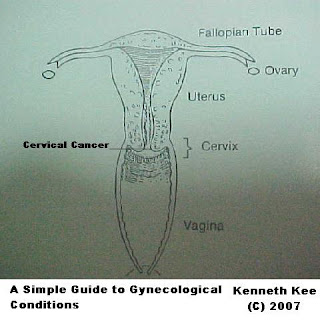
A Simple Guide to Cervical Cancer
--------------------------------------
What is Cervical Cancer?
------------------------------
Cervical cancer is a common cancer in women which affects the cervix (the neck of the womb).
What are the types of Cervical Cancer?
----------------------------
--------------------------------------
What is Cervical Cancer?
------------------------------
Cervical cancer is a common cancer in women which affects the cervix (the neck of the womb).
What are the types of Cervical Cancer?
----------------------------
There are 2 main types:
1. Squamous cell carcinoma
2. Adenocarcinoma
Squamous cell carcinorma is more common in the younger woman whereas the adenocarcinoma is more common in the older woman.
Who is at risk of Cervical Cancer?
---------------------------------------------
All women aged between 25 and 69 who had:
1. Sex intercourse at early age
2.Multiple sexual partners
3.Sexually transmitted infections (STI) e.g. genital herpes and human papillomavirus infection (HPV)
4.Any medical condition or treatment which affects the immune system eg. auti-immune disease
5.Smoking
What are the symptoms of cervical cancer?
---------- -----------------------------------------------
The following are symptoms of cervical cancer:
What are the symptoms of cervical cancer?
---------- -----------------------------------------------
The following are symptoms of cervical cancer:
1.Vaginal bleeding after sexual intercourse
2.Irregular bleeding in between periods or after menopause
3.Foul-smelling vaginal discharge
4.Non-specific pain in the pelvic area or lower back
5.Tiredness or loss of weight
The initial stages of cervical cancer are usually symptomless, so women may not know it.
Regular Pap smear screening detects abnormal changes in the cervical cells and prevents cancer.
How is Cervical Cancer Screening done?
-------------------------------------------------------
To check if you may have cervical cancer, go for a Pap smear test.
This is simple, quick, safe and is usually painless procedure.
If you have had sex before or are sexually active, you should go for a Pap smear once every 2 years.
Pap smears are available at all hospitals, most private clinics and the local Cancer Society.
If the Pap smear is positive, a colposcopy (examination of the inner lining of the womb) followed by cone biopsy of any suspicious area may be done.
What is the treatment of Cervical Cancer?
--------------------------------------------------------
In the pre-cancerous stage and Early Cancer Stage(carcinoma-in-situ) of the cervix, removal of all the abnormal tissues can be done by a cone biopsy.
The initial stages of cervical cancer are usually symptomless, so women may not know it.
Regular Pap smear screening detects abnormal changes in the cervical cells and prevents cancer.
How is Cervical Cancer Screening done?
-------------------------------------------------------
To check if you may have cervical cancer, go for a Pap smear test.
This is simple, quick, safe and is usually painless procedure.
If you have had sex before or are sexually active, you should go for a Pap smear once every 2 years.
Pap smears are available at all hospitals, most private clinics and the local Cancer Society.
If the Pap smear is positive, a colposcopy (examination of the inner lining of the womb) followed by cone biopsy of any suspicious area may be done.
What is the treatment of Cervical Cancer?
--------------------------------------------------------
In the pre-cancerous stage and Early Cancer Stage(carcinoma-in-situ) of the cervix, removal of all the abnormal tissues can be done by a cone biopsy.
Repeated Pap smears must be done to confirm that there is no recurrence of the cancer.
In all cases of established cancer of the cervix(stage II - IV), surgery is done with removal of the womb followed by radiotherapy( external or internal) and if necessary chemotherapy.
In all cases of established cancer of the cervix(stage II - IV), surgery is done with removal of the womb followed by radiotherapy( external or internal) and if necessary chemotherapy.
Reviews of the woman's condition is done regularly.
Sexual intercourse should be avoided temporarily after treatment.
Normal physical and social activities may be resumed in 2-3 month after treatment.
How do you prevent Cervical Cancer?
-------------------------------------------
A Pap smear screening test is the best prevention against Cervical Cancer.
A newly developed vaccine for HPV has been shown to be able to reduce the incidence of cervical cancer.
Avoid multiple sexual partners.
Use condoms for protection against sexually transmitted idsease especially HPV.
As usual keep a healthy lifestyle and have a well balanced diet
Sexual intercourse should be avoided temporarily after treatment.
Normal physical and social activities may be resumed in 2-3 month after treatment.
How do you prevent Cervical Cancer?
-------------------------------------------
A Pap smear screening test is the best prevention against Cervical Cancer.
A newly developed vaccine for HPV has been shown to be able to reduce the incidence of cervical cancer.
Avoid multiple sexual partners.
Use condoms for protection against sexually transmitted idsease especially HPV.
As usual keep a healthy lifestyle and have a well balanced diet
So take steps now to protect yourself against cancer.
Encourage your loved ones to go for screening if they have not done so.
Bear in mind that a pro-active approach with regular clinical screening is to prevent common cancers like breast and cervical cancers from affecting your lives.
Added 4th October 2008
---------------------------------
Cervical Cancer
---------------------
The most common HPV types causing 70% of all cervical cancers are the HPV 16,18, 31 and 45.
Both new vaccines against HPV Cervarix and Gardasil are equally effective in producing high antibodies against HPV 16 and 18 and preventing these infections over a 5 year period.
However prevention of the HPV 16 and 18 does not mean the cervical cancer can be abolished totally.
Subscribe to:
Posts (Atom)
Subscribe Now: Feed Icon
Clicktale
Labels
- abdominal pain (10)
- abnormal brain signals (1)
- abscess (1)
- Achilles tendinitis (1)
- acid reflux (2)
- acne (1)
- Acne Rosacea (1)
- Acoustic neuroma (1)
- Acquired Immune Deficiency Syndrome (1)
- acyclovir (2)
- ADDISON DISEASE (1)
- Adenoidectomy (1)
- Adenoiditis (1)
- Adenoids (1)
- Aedes mosquitoes (2)
- aerobics (1)
- aging (2)
- AIDS (2)
- air conditioners (1)
- alcohol (5)
- Alcoholism (1)
- allergens (2)
- allergies (1)
- allergy (2)
- alopecia (1)
- alzeheimer's disease (1)
- amblyopia (2)
- amebiasis (1)
- Amenorrhea (1)
- amylotrophic lateral sclerosis (1)
- anaemia (4)
- anaerobic bacteria (2)
- Anal fissure (1)
- Anal Fistula (1)
- analgesic (4)
- androgens (1)
- ANDROPAUSE (1)
- anger management (1)
- Angiogram (1)
- ankles (1)
- anopheles mosquito (1)
- anorectal abscess (1)
- anovulation (1)
- Answers (3)
- Anthrax (1)
- anti-aging (1)
- anti-diarrhoea (1)
- anti-flatulent (1)
- antibiotic (8)
- Antibiotic therapy (1)
- antibiotics (26)
- anticholinesterase (1)
- anticoagulant (1)
- antidepressant (1)
- antifungal (3)
- antihistamine (4)
- antimycotics (1)
- antioxidants (1)
- antispasmodic (2)
- Antispasmodics (1)
- antitoxins (1)
- antiviral (1)
- anus (2)
- anxiety (2)
- aphthous ulcers (1)
- Appendicitis (1)
- appendix perforation (1)
- appetite suppressant (1)
- areflexia (1)
- artane (1)
- Artery blockage (1)
- arthritis (4)
- articular cartilage injury (1)
- asbestos (1)
- aspiration (2)
- aspirin (1)
- asthma (1)
- Astigmatism (1)
- atherosclerosis (1)
- Athlete's Foot (1)
- atopic dermatitis (1)
- atopic eczema (2)
- atrial fibrillation (2)
- atrophic vaginitis (1)
- aural toilet (1)
- autoimmune disease (3)
- autoimmune neuromuscular disease (1)
- autonomic dysfunction (1)
- avitaminosis (1)
- avoid causative substance (1)
- avoid prolonged standing ulcers (1)
- avoid rubbing (1)
- avoid straining (1)
- avoid sudden movement (1)
- avoid touching the acne (1)
- axilla (1)
- back pain (1)
- Backache (2)
- Baclofen (1)
- bacteria (15)
- bacteria culture (4)
- bacterial (4)
- bacterial infection (6)
- bacterial vaginosis (1)
- bad posture (1)
- baking soda (1)
- Balanitis (1)
- ballooning (1)
- ballooning of blood vessel in brain (1)
- barking cough (1)
- bartholin cyst (1)
- basal cell carcinoma (1)
- Basal ganglia (1)
- bed bugs (1)
- bed sores (1)
- Bedding and clothing (1)
- bedwetting (2)
- bees (1)
- Beestings (1)
- Bence Jones (1)
- benign (3)
- Benign Prostatic Hyperplasia (1)
- Benzyl Benzoate lotion (1)
- Besy ahoo answer (1)
- beta blockers (1)
- biological targeted therapy. (1)
- biological warfare (1)
- biopsy (4)
- bipolar disorders (1)
- bipolar disorders treatment (1)
- bird flu (1)
- birth control (1)
- birth control methods (1)
- bladder cancer (3)
- bleeding (6)
- bleeding disorder (2)
- bleeding ulcers (1)
- Blepharitis (1)
- blindnes (1)
- blindness (4)
- blisters (3)
- bloating (5)
- blocked nose or ear (1)
- blocked opening of glands (1)
- Blood blockage (2)
- blood cancer (2)
- blood in sputum (1)
- blood in urine (2)
- blood loss (1)
- blood pressure (1)
- blood release (1)
- blood transfusion (2)
- bloodborne infection (1)
- blurred vision (4)
- BMI (1)
- bodyache (2)
- bone density test (1)
- bone fusion (1)
- bone infection (1)
- bone marrow transplant (3)
- bone pain (1)
- Bordetella pertussis (1)
- bowel movement (1)
- BPH (1)
- brace (1)
- bradyacardia (1)
- brain damge (1)
- brain infections (2)
- brain tumour (2)
- breast (1)
- breast cancer (1)
- breathless (6)
- brittle bones (1)
- broken blood vessels (1)
- Bronchitis (1)
- bronchodilator (2)
- bronchoscopy (1)
- bruise (1)
- BSE (1)
- Buerger's Disease (1)
- bulbar (1)
- burn calories (3)
- burning sensation (1)
- Burns (1)
- burrow lines on the skin (1)
- buttocks (1)
- CA 125 (1)
- calcium (1)
- calcium supplements (1)
- cancer (9)
- cancer of the cervix (1)
- cancer of vulva (1)
- Cancer screening (5)
- cancers (1)
- Candida albicans (2)
- Candidiasis (1)
- Carbamazepine (1)
- carbohydrate diet (1)
- cardiac tamponade (1)
- cardiogenic shock (1)
- cardiovascular collapse (1)
- cardioversion (2)
- Carpal Tunnel Syndrome (1)
- CAT Scan (1)
- cataract (1)
- Caudate nucleus (1)
- cautery (1)
- CD4 (T-cell) lymphocytes (1)
- Cellulitis (1)
- Central nervous system (1)
- cerebral aneurysm (1)
- cerebral palsy (1)
- cerebrovascular accident(CVA) (1)
- cervical cancer (2)
- Cervical Spondylosis (1)
- cervicitis (2)
- cervix cancer (1)
- cessation of menstruation (1)
- chalazion (1)
- changes in personality and behaviour (1)
- chemical treatment (1)
- chemicals (7)
- chemotherapy (10)
- chickenpox (2)
- chikungunya fever (1)
- child school problems (1)
- childhood (1)
- chills (1)
- Chlamydia (1)
- Cholecystectomy (1)
- Cholecystitis (2)
- Cholera (1)
- cholesterol (2)
- Choreia (disease) (1)
- choroid (2)
- chronic (4)
- chronic bronchitis (1)
- chronic fatigue (1)
- chronic illness (2)
- Chronic Obstructive Lung Disease (2)
- chronic pelvic pain. endometrosis (1)
- chronic suppurative otitis media (1)
- Cialis (1)
- cigarettes (1)
- ciliary body (1)
- ciprofloxacin (1)
- circumcision (1)
- cirrhosis.cold compress (2)
- cleaning (1)
- clofazimine (1)
- closed angle glaucoma (1)
- clusters (2)
- coccyx injury (1)
- cochlea (1)
- Coeliac Disease (1)
- cold compress (3)
- cold sores (1)
- cold temperatures (1)
- colic (1)
- collagen abnormalities (1)
- colon (1)
- colon cancer (1)
- colonoscopy (1)
- common (1)
- common cold (1)
- compression (2)
- compression of the median nerve (1)
- Conditions and Diseases (2)
- condoms (1)
- congenital (3)
- congenital deformities (1)
- congestion (1)
- congestive heart failure (1)
- conjuctivitis (2)
- conjuntiva (1)
- constipation (5)
- contact dermatitis (1)
- contact lens (4)
- contagious (1)
- contaminated food (2)
- contaminated soil (1)
- contaminated water and food (1)
- contents (1)
- contraction of the diaphragm (1)
- control diet (2)
- contusion (1)
- convulsions (1)
- cornea (1)
- corneal blockage (1)
- corneal ulcer (2)
- coronary artery bypass graft surgery (1)
- Coronary Heart Disease (1)
- corticosteroid creams (2)
- corticosteroid injections. (1)
- corticosteroids (3)
- cortisone injections (1)
- Corynebacterium diphtheriae (1)
- cough (7)
- CPAP (1)
- cramps (1)
- Crohn's Disease (1)
- crooked spine (1)
- Croup (1)
- CSF (1)
- curvature (1)
- CUSHING SYNDROME (1)
- cut (1)
- Cutaneous (1)
- Cutaneous Larva migrans (1)
- cystine (1)
- cystitis (1)
- cystoscopy (2)
- Cytomegalovirus (1)
- Dandruff (1)
- danger in pregnant mothers (1)
- danger of kidney and heart problems (2)
- dapsone (1)
- De Quarvian's Disease (1)
- deafness (3)
- decongestant (1)
- deep vein thrombosis (2)
- deformities (1)
- degree (1)
- dehydration (3)
- dementia (2)
- Demyelinating Diseases (1)
- dengue (1)
- Dengue Haemorrhagic Fever (1)
- Dengue Shock Syndrome (1)
- dental caries (1)
- dental hygiene (1)
- dental pain (1)
- Dental problems (1)
- depression (5)
- dermatophytes (1)
- desensitisation (1)
- diabetes (7)
- diabetes insipus (1)
- Diabetes Mellitus (2)
- dialysis (1)
- dialysis or transplant (1)
- diarrhea (6)
- diarrhoea (1)
- diastolic (1)
- diet (5)
- difficult breathing (1)
- diphenhydramine (1)
- Diphtheria (1)
- disability (1)
- discharge (1)
- discharge fom penis or vagina (1)
- dislocation of elbow (1)
- dislocation of shoulder (1)
- disorientation (1)
- diuretic (1)
- Diverticulitis (1)
- Diverticulosis (1)
- dizziness (1)
- dopamine transmitter (1)
- Down's Syndrome (2)
- drainage of pus (1)
- dribbling (2)
- drink more water (1)
- drug addict counselling (1)
- drug addicts (1)
- drugs (4)
- dry (3)
- drying agents (1)
- dryness (1)
- DTP vaccine (2)
- Duchenne (1)
- duchenne muscle dystrophy (1)
- DUPUYTREN'S CONTRACTURE (1)
- dust (3)
- dust mites (1)
- dysentery (2)
- Dysmenorrhea (1)
- dyspepsia (1)
- dysphagia (2)
- ear canal polyp (1)
- ear infections (1)
- ear pain (1)
- ear tugging (1)
- earache (1)
- earlobe infection (1)
- early 20 (1)
- eating disorders (1)
- ecchymosis (1)
- ECG (1)
- ectopic pregnancy (1)
- ECU tendonitis (1)
- Eczema (1)
- edema (1)
- elastic stockings (1)
- electricity (1)
- electrocardiogram (1)
- emergency (5)
- EMG (1)
- emotional (1)
- emphysema (1)
- encephalitis (3)
- endometrial tissues (1)
- Endometriosis (2)
- enlarged liver (1)
- enlarged liver and spleen (1)
- enlarged lymph nodes (2)
- enlarged neck nodes (1)
- enlarged tonsils (2)
- enlarged uterus (1)
- entecavir (1)
- enteric virus (1)
- Entropion (1)
- enuresis (2)
- Epididymitis (1)
- epiglottis flip backwards (1)
- epilepsy (1)
- epistaxis (1)
- Epstein-Barr virus (3)
- Erectile dysfunction (1)
- erosions (1)
- erythrodermic (1)
- erythromycin (1)
- essential (1)
- eustachian tubes (1)
- excess thyroid hormones (1)
- Excessive Menstrual Bleeding (1)
- excessive use of voice (1)
- excessive vaginal bleeding (1)
- exercise (8)
- extent (1)
- eye (1)
- eye injuries (1)
- eye ointment (1)
- eye pain (1)
- eye protection (1)
- eye strain (1)
- eyedrops (2)
- eyelashes (1)
- eyepads (1)
- eyes (1)
- facial massage (1)
- facial palsy (1)
- family history (2)
- Family Medical Doctor (40)
- fast growing (1)
- fast heart beat (1)
- fast heartbeats (1)
- fat absorption suppressant (1)
- fatigue (2)
- fear (1)
- female hormones (1)
- female predominance (1)
- fever (22)
- fiber (1)
- fibrates (1)
- fibre (1)
- fibroid (1)
- fibroids (1)
- Fibromyalgia (2)
- fibrosis (1)
- fibrous tissue (2)
- filiform (1)
- Finasteride (1)
- finger nails (1)
- fish skin (1)
- fits (1)
- flat foot (1)
- fluid (1)
- fluids (3)
- foetal development (1)
- folic acid (1)
- folic acid deficiciency (1)
- Folliculitis (2)
- food allergy (1)
- food triggers (1)
- Foot and Mouth Disease (1)
- Foot care (2)
- footwear (1)
- foreign bodies (2)
- forgetfulness (1)
- fracture (1)
- fractures (2)
- frequency (4)
- frequent cystitis (1)
- frequent urine (1)
- Frozen Shoulder (1)
- full stomach (1)
- functional (1)
- functional disorder (1)
- fungal (4)
- fungi infection (1)
- fungus (1)
- fungus Malassezia furfur (1)
- fusion (1)
- g6pd deficiency (1)
- Gait abnormality (1)
- gallbladder (1)
- gallbldder (1)
- gallstone (1)
- gallstones (1)
- ganglion (1)
- ganglion cyst (1)
- gangrene (2)
- gas (1)
- gastritis (2)
- gastroscopy (2)
- generalised rash (4)
- genes (2)
- genetic (8)
- genetic factor (2)
- genetics (1)
- Genital Herpes (1)
- genital warts (1)
- gerd treatment (2)
- german measles (1)
- Gestational diabetes (1)
- giant cell arteritis (1)
- giardiasis (2)
- giddiness (1)
- giddy (1)
- Gingivitis (1)
- glans (1)
- glass (1)
- glaucoma (1)
- Glomerulonephritis (1)
- Glossitis (1)
- Gluten Enteropathy (1)
- goiter (1)
- good dental hygiene (1)
- good posture (1)
- gout (1)
- gradual onset (1)
- gram negative bacteria (1)
- gram positive (1)
- grand mal (1)
- grayish tonsillar exudate (1)
- groins (1)
- Guillain-Barre Syndrome (1)
- gum boils (1)
- guttate (1)
- gynecologic cancer (1)
- gynecological cancer (1)
- Gynecomastia (1)
- hair follicles (1)
- hair loss (1)
- hair transplant (1)
- hair weaving (1)
- Halitosis (1)
- hallux vulgus (1)
- halos (1)
- Hand (1)
- hand hygiene (1)
- hard large stools (1)
- harden stools (1)
- hasty swallowing of food or air (1)
- HBV virus infection (1)
- HCV (1)
- HCV antibodies (1)
- HDL (1)
- head injury (2)
- headache (10)
- Health (1)
- Health education (2)
- health issues (1)
- healthy life stye (1)
- healthy lifestyle (6)
- hearing loss (1)
- heart (1)
- heart attack (1)
- heart disease (1)
- heartburn (2)
- heat (1)
- Heat Stroke (1)
- heel pads (1)
- Helicobacter pylori (2)
- heliobactor pylori (1)
- helpless (1)
- hemophilia (1)
- hemorrhage (1)
- HENOCH-SCHONLEIN PURPURA (2)
- Hepatitis (1)
- Hepatitis A (1)
- hepatitis A virus(HAV) (1)
- hepatitis B (2)
- Hepatitis C (1)
- hepatitis virus (1)
- hepatitis. (2)
- hepatocytes (1)
- herald patch (1)
- hereditary (7)
- herniorrhaphy (1)
- herpes virus (1)
- herpes zoster (1)
- hiatus hernia (1)
- hiccup (1)
- high blood pressure (1)
- high cholesterod (1)
- high cholesterol (1)
- high level (1)
- high mortality (2)
- high protein food (1)
- hips (1)
- histamine (1)
- HIV (2)
- HMB-45-positive (1)
- HMF (1)
- holes (1)
- hormonal (2)
- hormonal imbalance (1)
- hormone (3)
- Hormone replacement therapy (1)
- hormone treatment (1)
- hornets (1)
- hot flushes (1)
- HPV (1)
- HPV DNA test (1)
- HRT (1)
- HSV1 (1)
- HSV2 viruses (1)
- Human Immunodeficiency Virus (1)
- Human papilloma virus Infection (1)
- human papillomavirus (2)
- Huntington (1)
- Huntington's disease (1)
- Hydrocoele (1)
- hypercalcemia (1)
- hyperextended knees (1)
- Hyperhidrosis (1)
- HYPERKALEMIA (1)
- hypernatremia (1)
- hyperparathyroidism (1)
- Hypertension (4)
- Hyperthyroid Disease (1)
- hypnotherapy (1)
- hypocalcemia (1)
- hypokalemia (1)
- hyponatremia (1)
- hypoparathyroidism (1)
- hypothyroid (1)
- hypothyroidism (1)
- hysterectomy (1)
- i/v fluids (1)
- Ichthyosis (1)
- IgM antibodies (1)
- immature blood cells (1)
- immunosuppressant (1)
- immunotherapy (2)
- Impetigo (1)
- incised and drained (1)
- index by labels (1)
- infected crust (2)
- infected oil gland (2)
- infection (4)
- infection. hair follicle (1)
- infections (7)
- infectious (3)
- Infectious Mononucleosis (1)
- infertility (3)
- infertility. (1)
- inflammation (7)
- inflammation of airway (1)
- inflammation of the mouth (1)
- influeza (3)
- infranuclear (1)
- Inguinal hernia (1)
- inhalation (1)
- inherited (1)
- inherited blood clotting (1)
- injection (1)
- injuries (1)
- injury (8)
- insects (1)
- insomnia (1)
- insufficient blood flow (1)
- insufficient haemaglobin (1)
- insulin (2)
- interferon (1)
- intermittent claudication (1)
- Intertrigo (1)
- intestinal (2)
- intestinal perforation (1)
- intestines (1)
- intraocular pressure (1)
- intrauterine device (1)
- intussusception (1)
- invasive (2)
- inverse (1)
- iris (1)
- iron (1)
- irregular meals (1)
- irregular menses (1)
- irregular rhythm (1)
- Irritable Bowel Syndrome (1)
- irritants (1)
- irritation (1)
- isorbide (1)
- itch (6)
- Itchiness (1)
- itching (2)
- itchy (2)
- itchy nose (1)
- IUD (1)
- jaundice (5)
- joint pain (1)
- joints (2)
- KAWASAKI DISEASE (1)
- keloid (1)
- kidney (2)
- Kidney cancer (1)
- kidney damage (1)
- kidney disease (3)
- Klinefelter's Syndrome (1)
- Knee cap dislocation (1)
- knee ligaments injury (1)
- knee Xray (1)
- knees (1)
- knock (1)
- Koplik's spots (1)
- laceration (1)
- lactobacillus bacteria (1)
- laminectomy (1)
- lamivudine (1)
- laparoscope (1)
- lapband (1)
- Laryngeal cancer (1)
- Laryngitis (1)
- laryngopharyngeal reflux (1)
- Laryngx (1)
- laser (1)
- laser coagulation (1)
- laser surgery (1)
- LASIK (1)
- LASIK surgery (1)
- late teen (1)
- latent (1)
- LDL (1)
- leg (1)
- Legionnaire's Disease (1)
- lens transplant (1)
- leprosy (1)
- leptospirosis (2)
- leucocytosis (1)
- leukemia (1)
- levadopa (1)
- Levitra (1)
- Lice (1)
- lichen planus (1)
- life threatening (1)
- lifelong (2)
- ligamentous sheath (1)
- light sensitivity (1)
- limping (1)
- lipids (1)
- lipoma (1)
- liposarcoma (1)
- liposuction (1)
- Little's area (1)
- liver (1)
- liver cancer (3)
- Liver Cirrhosis (2)
- liver dysfunction. (1)
- Longo technique (1)
- loose ligaments (1)
- lose weight (3)
- loss in life events (1)
- loss of appetite (3)
- loss of memory (1)
- loss of mobilty (1)
- lots of water (1)
- low calcium (1)
- low fibre (1)
- low level (1)
- low oestrogens (2)
- low platelets (1)
- low thyroid (1)
- low Vitamin D (1)
- lower abdominal cramp (1)
- lower abdominal pain (1)
- lower immunity (1)
- lumbar spinal stenosis (1)
- lump (1)
- lump in neck (1)
- lung cancer (2)
- lymph node enlargement (1)
- lymph nodes (2)
- lymphatic system (1)
- lymphocytes (1)
- lymphoma (2)
- M proteins (1)
- Magnetic resonance imaging (1)
- maic attacks (1)
- major cosmetic surgery (1)
- malaria (1)
- Malathion 0.5% lotion (1)
- male baldness (1)
- MALE MENOPAUSE (1)
- malignant (3)
- mammogram (1)
- mandibular branches (1)
- marfan's syndrome (1)
- massage therapy (1)
- mast cells stimulant (1)
- Mastitis (1)
- maxillary (1)
- McBurney's Point (1)
- measles (2)
- Medical case Studies (125)
- medical conditions (5)
- medication side effects (2)
- medications (3)
- medicine (1)
- medicines (2)
- meditation (2)
- megacolon (1)
- melanin (1)
- melanoma (1)
- memory loss (1)
- men (1)
- Meniere's Disease (1)
- meningitis (2)
- meningococcus (1)
- meniscus tears (1)
- menopause (3)
- menorrhagia (3)
- mental illness (1)
- mental retardation (1)
- metal (1)
- methotrexate (1)
- metronidazole (1)
- migraine (1)
- mild fever (1)
- mildly contagious (1)
- minoxidil (1)
- miscarriage (1)
- MMR vaccine (3)
- moist (1)
- moisturizer (1)
- MOLLUSUM CONTAGIOSUM (1)
- mood changes (1)
- mood swings (1)
- motivation (1)
- motor disabilities (1)
- motor neurone disease (1)
- mouth (1)
- mouth ulcers (3)
- mouth washes (1)
- moving tract (1)
- MRI (5)
- multibacillary (1)
- multiple myeloma (2)
- Multiple sclerosis (1)
- mumps (2)
- Murphy Sign (1)
- muscle (3)
- muscle relaxant (1)
- muscle relaxant (6)
- muscle spasm (1)
- Muscle Tension Dysphonia (1)
- muscle weakness (1)
- music therapy (1)
- mutate (1)
- myasthenia gravis (1)
- mycobacterium leprae (1)
- Myelin (1)
- myocarditis (1)
- narrowed disc space (1)
- narrowed foramina (1)
- narrowing of artery (1)
- narrowing of bronchi (1)
- nasal congestion (1)
- nasal packing (1)
- nasal polyp (1)
- nasal spray (1)
- Nasopharyngeal cancer (2)
- nasopharynx (1)
- natural (1)
- nausea (5)
- neck collars (1)
- neck rigidity. (1)
- Neisseria gonorrhoeae (1)
- NEPHROTIC SYNDROME (1)
- nerve cells (1)
- nerve compression (1)
- nerve conduction test (1)
- neurological deficit (1)
- Neurological Disorders (1)
- neurotransmission (1)
- new bone (1)
- new drugs (1)
- niacin (1)
- Night Blindness (1)
- nitrosamines (1)
- Nits on scalp (1)
- no cure (1)
- no menstruation (1)
- no petechiae (1)
- nocturia (4)
- non-paralytic (1)
- non-small cell (1)
- Normal Pressure Hydrocephalus (1)
- nose (1)
- nosebleed (2)
- NSAID (1)
- NSAIDS (3)
- numbness (1)
- Obesity (5)
- Obesity.frequent thirst (1)
- obstruction (1)
- obstruction to air flow (1)
- Obstructive Sleep Apnea (1)
- odor (1)
- older adults (1)
- olecranon bursitis (1)
- open angle glaucoma (1)
- open sores (1)
- optic nerve (1)
- or penis (1)
- oral (1)
- oral diabetic medicine (1)
- oral hygience (1)
- orchitis (2)
- Osteogenesis Imperfecta (1)
- osteomalacia (1)
- Osteomyelitis (1)
- osteophytes (1)
- osteoporosis (4)
- otitis externa (1)
- otitis media (3)
- Ovarian cancer (2)
- Ovarian torsion (1)
- overactivity (1)
- overflow (1)
- overweight (1)
- oxalates (1)
- P.falciparium (1)
- P.malariae (1)
- P.ovale (1)
- P.vivax (1)
- pain (25)
- painful (3)
- painful fallopian tubes (1)
- painful menstruation (1)
- painful swollen parotid glands (1)
- painful urination (1)
- painkillers (10)
- palms (1)
- pancreatic cancer (1)
- pancreatitis (4)
- panic attacks (1)
- Papanicolaou tests Pap smear (1)
- paralysis (2)
- paralytic (1)
- parasite (1)
- parasitic (1)
- Parkinson (1)
- paromyxovirus (1)
- Paronychia (1)
- partial (1)
- paucibacillary (1)
- PECOMA (1)
- Pediculosis (1)
- peduncle (1)
- pelvic inflammatory disease (3)
- pelvic pain (2)
- pelvis (1)
- Penicillin (1)
- penile implants (1)
- penile injection (1)
- penis (2)
- peptic ulcer (1)
- perforation (1)
- Pericarditis (1)
- peritonitis (1)
- Perivascular epithelioid cell (1)
- permanent disability (1)
- Permethrin 1% cream rinse (1)
- perpheral neuropathy (1)
- persistant cold (1)
- persistent pain (1)
- pessaries (1)
- petit mal (1)
- Phalen's test (1)
- phenytoin (1)
- phlebectomy (1)
- phlebitis (1)
- phlegm (1)
- photodermatitis (2)
- phototherapy (1)
- physiotherapy (7)
- physiotheray (1)
- PID (2)
- pigmentation (1)
- piles (2)
- pimples (1)
- pityriasis capitis (1)
- Pityriasis Rosea (1)
- plane (1)
- plantar (1)
- plantar fascilitis (1)
- plaque (1)
- plasma cell (1)
- plasmapheresis (1)
- Plasmodium (1)
- Pleural Effusion (1)
- pleurodesis (2)
- pneumococcus (2)
- pneumonia (2)
- Pneumothorax (1)
- polio virus (1)
- Poliomyelitis (1)
- pollen (2)
- Polycystic kidney disease (1)
- polycystic ovarian syndrome (1)
- polycystic ovary (2)
- polyps (3)
- poor blood circulation (1)
- poor coordination (1)
- poor drainage (1)
- poor healing of skin (1)
- porphyria (1)
- post-herpetic neuralgia (1)
- Postmenopausal bleeding (1)
- pregnancy (7)
- preinvasive (1)
- Premature (1)
- Premenstrual syndrome (1)
- prepuce (1)
- preserved food (2)
- pressure and posture (1)
- pressure change (1)
- pressure on nearby organs (1)
- Prickly Heat (1)
- prickly sensation (1)
- Primary (3)
- primary health care (1)
- probe (1)
- proctocolectomy (1)
- progressive disease (1)
- prolapsed disc (1)
- prolapsed intervertebral disc (1)
- prostate (6)
- prostate cancer (1)
- prostatic fluid test. bacteria culture (1)
- Prostatitis (1)
- Protease inhibitors (1)
- protozoan (1)
- pruritus (1)
- pseudocysts (1)
- pseudomembraous enterocolitis (1)
- pseudomonas (1)
- psoriasis (1)
- psychological factor (1)
- psychological suffering (1)
- Pterygium (1)
- puberty (1)
- pulmonary embolism (1)
- purpura (1)
- pustular (2)
- pustule (1)
- pyloric stenosis (1)
- quality of life (1)
- quinines (1)
- radiation (4)
- radioactive iodine (1)
- radiofrequency ablation (1)
- radiotherapy (9)
- radiotherapy. (1)
- rare (1)
- rash (2)
- rashes and abrasions (1)
- Raynaud's Disease (1)
- rectum (1)
- recurrence (1)
- recurrent outbreaks (1)
- red (5)
- red eyes (2)
- red scaly patches (1)
- redness (2)
- reduced oxygen (1)
- reflex mechanism (1)
- regenerated cells (1)
- regenerated tissue (1)
- region (1)
- regional enteritis (1)
- Regular checkups (1)
- rehyration (1)
- reiki (1)
- relax (2)
- relaxation (1)
- relaxation techniques (1)
- renal failure (1)
- renal stones (1)
- reorganisation (1)
- rest (12)
- rest tremors (2)
- rest voice (1)
- retention of urine (1)
- retina (1)
- retinal detachment (1)
- Retinitis pigmentosa (1)
- Reverse transcriptase (RT) inhibitors (1)
- Reye's syndrome (1)
- rheumatoid arthritis (1)
- rhinitis (1)
- rice water diarrhoea (1)
- rifampicin (1)
- rigidity (1)
- rigors (1)
- rose spots (1)
- roseala infantum (1)
- rotablation (1)
- rotator cuff injuries (1)
- rubber band (1)
- rubella (1)
- rule of nines (1)
- runny nose (2)
- sad (1)
- Salivary Gland cancer (1)
- salivary glands (1)
- Salmonella typhi (1)
- Salpingitis (1)
- Sarcoptes Scabiei (1)
- scabicides (1)
- Scabies (1)
- Scalds (1)
- scarlet fever (2)
- schizophrenia (1)
- sciatic nerve (1)
- sciatica (3)
- sclerotherapy (1)
- scoliosis (1)
- scratch marks (1)
- scratching (1)
- scurvy (1)
- sebaceous glands (2)
- seborrheic (1)
- secondary (5)
- seizures (1)
- semen.PSA (1)
- sentinel pile (1)
- septic arthritis (1)
- septicemia (1)
- severe and prolonged joint pains (1)
- Sex linkage (1)
- sexual activity (1)
- sexual contact (1)
- sexual exposure (1)
- Sexual Health (1)
- sexually transmitted disease (9)
- shampoo (1)
- sharp object (1)
- shigella (1)
- shingles (1)
- shivering (1)
- shock (1)
- Shoulder Xray (1)
- shunt (1)
- silent killer (1)
- silvadene (1)
- simple guide (2)
- simple skin care (1)
- single (1)
- sinus blockage (1)
- sinus washout (1)
- sinuses (1)
- sinusitis (2)
- skin (13)
- skin disease (1)
- skin Polyp (1)
- skin rash (1)
- Skin scrapings (1)
- skin tags (1)
- skin trophi (1)
- sleeping sickness (1)
- slipped disc (1)
- slow development (1)
- slow movement (1)
- slow urine flow (1)
- small cell (1)
- small papules (1)
- Small red bites (1)
- small vesicle (1)
- smoking (12)
- sneezing (2)
- snoring (2)
- soaps (1)
- socks (1)
- sodium valproate (1)
- soles (1)
- sore throat (4)
- sorethroat (1)
- Spasmodic (1)
- spasticity (1)
- spectacles (1)
- speech (1)
- speech loss (1)
- spine (1)
- Spine Xray (2)
- spleen (1)
- sponging (1)
- Spontaneous (1)
- spontaneous abortion (1)
- spore forming bacterium (1)
- spread (1)
- squamous cell carcinoma (1)
- staphalococcus aureus (1)
- staphylococci (1)
- staphylococcus aureus (1)
- statins (1)
- STD (2)
- stem cells (3)
- stent (1)
- stepladder fever (1)
- steroid (2)
- Steroid or immunosuppressive drugs (1)
- steroids (3)
- stiffness (3)
- stinger (1)
- stitching (1)
- stomach cancer (1)
- stomach inflammation (1)
- Stomatitis (1)
- stones (1)
- stool blood test (2)
- stool softener (1)
- stools (1)
- stop itch and pain (1)
- strangulated hernia (1)
- streptococci (1)
- streptococcus (1)
- stress (14)
- stridor (1)
- stripping of veins (1)
- stroke (5)
- stye (1)
- Subarachnoid Hemorrhage (1)
- subclinical (1)
- suicide (1)
- sulfasalazine (2)
- sulphonamides (1)
- sun (1)
- sun exposure (2)
- superficial (1)
- superficial linear tear (1)
- supranuclear (1)
- sur (1)
- surgery (33)
- surgery. (1)
- surgical coning of cervix (1)
- surgical resection (1)
- sweat glands (1)
- sweet urine (1)
- swelling (6)
- swelling in abdomen (1)
- swollen blood vessels (1)
- swollen glands behind ears and neck (1)
- sympathectomy (1)
- symptomatic treatment (1)
- syncope (1)
- Syphilis (1)
- Systemic Lupus Erythematosis (1)
- systolic (1)
- tachycardia (1)
- tamoxifen (1)
- tears (1)
- telbivudine (1)
- temperature change (2)
- tender (1)
- tennis elbow (2)
- Tenosynovitis (1)
- tension (2)
- Tertiary (1)
- testicular pain (1)
- Testicular torsion (1)
- testosterone (1)
- tetanus (1)
- tetanus toxoid vaccine. Triple Antigen (1)
- tetracycline (2)
- thalassaemia (1)
- Thalassemia (1)
- thenar muscle wasting (1)
- Threadmill (2)
- threadworms (2)
- thymectomy (1)
- thymus (1)
- thyroid nodules (2)
- thyroid scan (1)
- thyroxine (1)
- tic (1)
- tinnitus (4)
- tinnitus. (1)
- tiredness (1)
- tissue damage (1)
- toe nails (1)
- tonsils (1)
- tooth discoloration (1)
- toothache (1)
- torsion (1)
- tracheostomy (2)
- track (1)
- traction (1)
- tranexamic acid (1)
- Transient ischaemic attack(TIA) (1)
- trauma (2)
- Treponema pallidum (1)
- Trichomonas vaginalis (1)
- trichomoniasis (1)
- trigeminal nerve (1)
- Trigeminal Neuralgia (1)
- trigger finger (1)
- trigger points (2)
- triggers (2)
- triglycerides (1)
- trimesters (1)
- tropical sprue (1)
- trypanosomes (1)
- tumour (1)
- Turner Syndrome (1)
- TURP (1)
- tying (1)
- Type 1 (1)
- Type 2 (1)
- typhoid carrier (1)
- Typhoid Fever (1)
- ueteric stones (1)
- Ulcerative Colitis (1)
- ulcers (2)
- ultrasound (4)
- ulttasound (1)
- UNDESCENDED TESTES (1)
- unknown cause (1)
- unwashed hands (1)
- urate crystals (1)
- ureteric colic (1)
- urethitis (1)
- Urethritis (1)
- urge (1)
- urgency (1)
- uric acid (1)
- uric aid (1)
- urinary incontinence (1)
- Urinary stones (1)
- Urinary Tract infection (1)
- urine problem (1)
- urine test (3)
- urostomy (1)
- urticaria (2)
- uterine ablation (1)
- uterine causes (1)
- Uterine Fibroids (1)
- uterine prolapse (1)
- uterus prolapse (1)
- UV light (1)
- uvea (1)
- uveitis (2)
- vaccine (2)
- vagina (2)
- vagina cancer (1)
- vaginal cancer (1)
- vaginal changes (1)
- vaginal discharge (1)
- vaginal douche (1)
- vaginal soreness (1)
- varicella vaccine (1)
- varicella-zoster virus (1)
- Varicose Veins (1)
- vasomotor rhinitis (1)
- vegetarian (1)
- venogram (1)
- venous stasis (1)
- vermiform appendix (1)
- vertigo (2)
- vertigo. (1)
- vesicovaginal fistula (1)
- Viagra (1)
- Vibrio cholorae (1)
- Vincent's Angina (1)
- viral (12)
- viral infection (2)
- viral infections (1)
- virus (3)
- viruses (1)
- vision loss (2)
- Vitamin A analogues (1)
- Vitamin A Deficiency (1)
- vitamin B1 deficiency (1)
- Vitamin B12 (1)
- Vitamin B12 Deficiency (1)
- Vitamin B2 Deficiency (1)
- vitamin B3 deficiency (1)
- vitamin B5 deficiency (1)
- Vitamin B6 Deficiency (1)
- vitamin B7 deficiency (1)
- Vitamin Bs (1)
- vitamin C deficiency (1)
- Vitamin D (1)
- Vitamin E Deficiency (1)
- vitamin K (1)
- Vitiligo (1)
- vitrectomy (1)
- vocal cord cyst (1)
- vocal cord nodule (1)
- vocal cord polyp (1)
- vocal cords (1)
- vocal paralysis (1)
- voice change (1)
- vomiting (5)
- vulva (1)
- Vulvitis (1)
- wafarin (1)
- walking (1)
- warm water (1)
- warmth (1)
- warts (1)
- wash hands (1)
- wash with water (1)
- wasps (1)
- wax (1)
- weak immune system (1)
- wear and tear (1)
- webs toes of foot (1)
- weight loss (7)
- Whooping cough (1)
- Wickham's striae (1)
- Widal test (1)
- wigs (1)
- wounds (1)
- wrist splintage (1)
- wrists (1)
- X-rays (3)
- xeroderma pigmentosa (2)
- yellow fever (1)
- yellow-green vaginal discharge (1)
- yoga (1)
- young child (1)




